This is a guest post by Maggie Helliwell, retired English general practitioner and former Vice Chair of NICE. See also Part 1.
We visited five different types of primary care health clinics, one in central Hanoi and four in the provinces and villages. They were immaculately clean, reasonably well-appointed facilities – with good basic equipment including simple laboratory machines, ultrasound, x-ray, slit lamps, dental chairs, small pharmacies, a room for traditional medicine, herbs and acupuncture and rooms for minor injuries and minor surgery – and appeared to be reasonably staffed by passionate and dedicated workers.
However, there were very few patients in evidence, in marked contrast to my practice in Keighley (northern England) serving a similar population. They were seeing 50 people a week where I was seeing up to 30-60 a day with my partners, and a large team seeing 30 people a day each in up to 10 different rooms. This contrast was stark. The staff were absolutely passionate and knowledgeable at the changes they perceived needing to be made – they knew that with the right support they could offer a good service to their population and talked to us about their understanding of the obstacles in their way. One is that home visits are not covered by health insurance, which is a great barrier in managing their increasing ageing population. Currently the Vietnamese population can opt out of family medicine clinics and chronic disease management, and use their health insurance on a symptom-by-symptom presentation at the hospital and the majority choose to exercise that right.
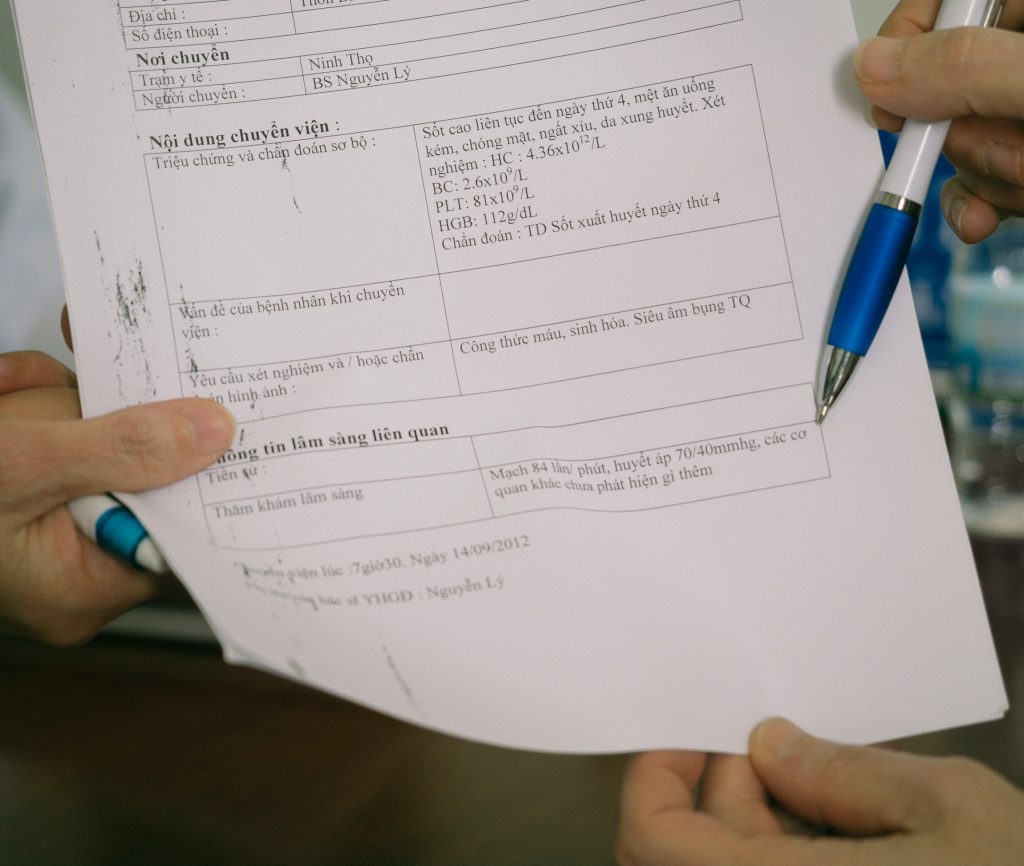
Proforma for patient referrals from primary care, at a primary healthcare pilot site in Khanh Hoa province
The doctors were all requesting better methods of communication and record keeping – very often there was no computer or only one computer which was used for health insurance management.. They did understand about paper record keeping and had excellent proformas, and used email and mobiles to communicate with their hospital counterparts, but they all felt this could be improved.

Dr Yongyuth Pongsupap (National Health Security Office, Thailand) sharing the lessons from Thailand on ‘matrix’ team working between district hospitals, village health centres, and families, for effective primary care
The week led up to a day long workshop chaired by the Vice Minister of Health, Prof Pham Le Tuan, and convened by the Health Strategy and Policy Institute (HSPI). We made our presentations and then heard from the Vietnamese delegates. The floor was then opened to all for discussion, and delegate after delegate got up and spoke about their perceptions and their solutions. There were multiple points of view and a lively debate, but the Vice Minister made it clear that primary care is going to be developed, that there were potentially many solutions, they knew they had to modify the health insurance system as a lever for progression, and that it would take time. Vietnam is already trying pilots of new primary care in some provinces, and I advised them to evaluate those pilots properly before proceeding to the next steps, something we are not very good at in England.
 Discussion chaired by Prof Pham Le Tuan (Vice Minister of Health), Mr Nguyen Minh Thao (Deputy Director of Vietnam Social Security), and Dr Maggie Helliwell
Discussion chaired by Prof Pham Le Tuan (Vice Minister of Health), Mr Nguyen Minh Thao (Deputy Director of Vietnam Social Security), and Dr Maggie Helliwell
The week culminated in a dinner with the Vice Minister in an outdoors restaurant overlooking the bay in Nha Trang. The dinner reflected the healthy Vietnamese diet I had experienced all week. A great deal of fresh fish and shellfish, and some meat accompanied by fresh vegetables and noodles or rice, followed by chunks of beautiful fresh fruit, watermelon and pineapple. A satisfying end to a very interesting and illuminating week.